It's been almost six weeks since the day we were told, "Mason's X-ray is not normal". Mason started having pain in his hip on a Sunday evening and by the next morning his pain was so severe he couldn't move without yelling out in pain. We took him in to our pediatrician thinking that maybe he had sprained his hip during his busy weekend of soccer, jumping on the trampoline and playing on the jungle gym at church. He had an x-ray and we were told there were possible signs of avascular necrosis (AVN) but we would need to wait 10 days to have a repeat X-ray before we would know for sure. It could be AVN or there was also a possibility it was a tumor or an infection. My heart was so broken. My precious boy had already been through so much in his life. I had such an overwhelming feeling of: "This isn't fair." I wanted to yell at God and tell him: Not my Mason. Pick someone else for this. He deserves better than this. More than this. I felt like I could cry an ocean of tears. I pleaded with God to do a miracle and heal our sweet boy. Ten days passed and we had another X-ray. The radiologist and the doctor gave us the news, "He most likely has Perthes disease."
Legg-Calvé-Perthes disease (LCPD) is a form of osteonecrosis of the hip that is found only in children. Mason looks totally healthy on the outside, but on the inside, his bone is dying. Part of me felt relief knowing that it probably wasn't a tumor or the "C" word. But the Perthes diagnosis felt heavy. Mason could no longer play soccer. No more jumping on the trampoline. No recess. No P.E. No jungle gym. No more playing on his scooter. How would we tell our 5 year old that he can't do all of his favorite things any more?
It's so incredibly painful to see Mason's soccer cleats sitting in our garage. We bought them in a bigger size so he could wear them for more than a season of soccer. Every time I look at them I'm reminded that he will never wear them again and I won't see him running up and down the soccer field again.
Seeing other kids running and jumping feels like being punched in the stomach. Driving by our pediatrician's office makes my heart ache. We used to be able to handle all of our problems there. Get an antibiotic, get a shot, get a sucker. Little problems. But this, it felt so big. We're now seeing an orthopedic surgeon at Children's hospital. We're talking about surgery and we're talking about a wheelchair. I feel like I'm living a life parallel to the one I expected. I'm grieving the loss of that other life. The one where Mason is still playing soccer. The one where he can run and jump and play with the other kids and he doesn't have to sit alone in the office at school during recess.
Legg-Calvé-Perthes disease (LCPD) is a form of osteonecrosis of the hip that is found only in children. Mason looks totally healthy on the outside, but on the inside, his bone is dying. Part of me felt relief knowing that it probably wasn't a tumor or the "C" word. But the Perthes diagnosis felt heavy. Mason could no longer play soccer. No more jumping on the trampoline. No recess. No P.E. No jungle gym. No more playing on his scooter. How would we tell our 5 year old that he can't do all of his favorite things any more?
It's so incredibly painful to see Mason's soccer cleats sitting in our garage. We bought them in a bigger size so he could wear them for more than a season of soccer. Every time I look at them I'm reminded that he will never wear them again and I won't see him running up and down the soccer field again.
Seeing other kids running and jumping feels like being punched in the stomach. Driving by our pediatrician's office makes my heart ache. We used to be able to handle all of our problems there. Get an antibiotic, get a shot, get a sucker. Little problems. But this, it felt so big. We're now seeing an orthopedic surgeon at Children's hospital. We're talking about surgery and we're talking about a wheelchair. I feel like I'm living a life parallel to the one I expected. I'm grieving the loss of that other life. The one where Mason is still playing soccer. The one where he can run and jump and play with the other kids and he doesn't have to sit alone in the office at school during recess.
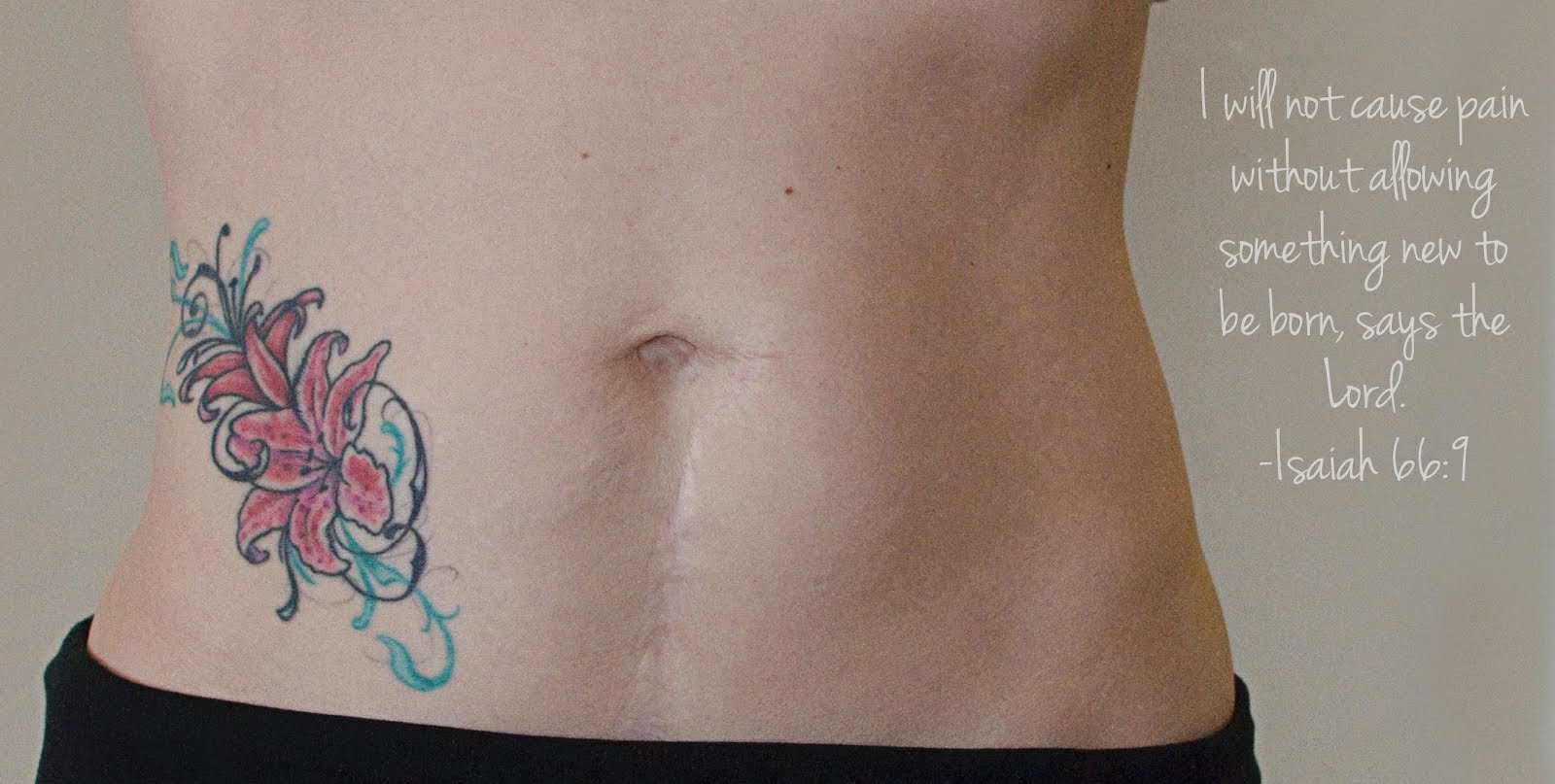
I'm still working on accepting this new normal. I came across a picture of Mason and I from 6 weeks ago. It was taken the day before Mason's diagnosis. I look at myself in the picture and I think, "You have no idea. You're world is about to be turned upside down." That woman in the picture is so naïve. That woman in the picture thought that infertility and the complications that's followed- that was the big struggle. The big struggle was over and now all we needed to worry about were the daily struggles of having 3 kids. Tantrums and juggling schedules, mountains of laundry and dishes that fill the sink.
Last week I got an email from Mason's teacher. She mentioned that Mason had been discouraged because he couldn't join the other kids in an activity. He told her, "I never get to do anything anymore." It was a hard day. There have been so many of those lately. I don't want my sweet boy to feel left alone and left out. So I talked to the school and now Mason gets to bring a friend with him to the office to play with Legos during recess. The first day he was so incredibly happy that he didn't have to sit by himself while the other kids played outside. He was smiling ear to ear when I picked him up from school. I emailed his teacher to tell her how happy I was to see a smile on his face. In her response email his teacher said, "Yay for small victories!!" I've been thinking of that each day. Celebrating the small victories. If I've learned anything in the last 6 weeks it is that. The challenges and the unknown seem so daunting but I celebrate those small victories like never before.
I know that I serve a good God. The same God who I prayed to every night as we struggled through our infertility and through complications and surgeries. And He is the same God who gave us our precious miracle, Mason. We're praying Mason makes a full recovery. We're praying for strength and courage because this journey may take many years. For now we will take it one day at a time and we will celebrate each and every small victory.
Mary Ann
Mary Ann